Get the Facts: Why Choose Cannabis Over Opioids to Address Chronic Pain?
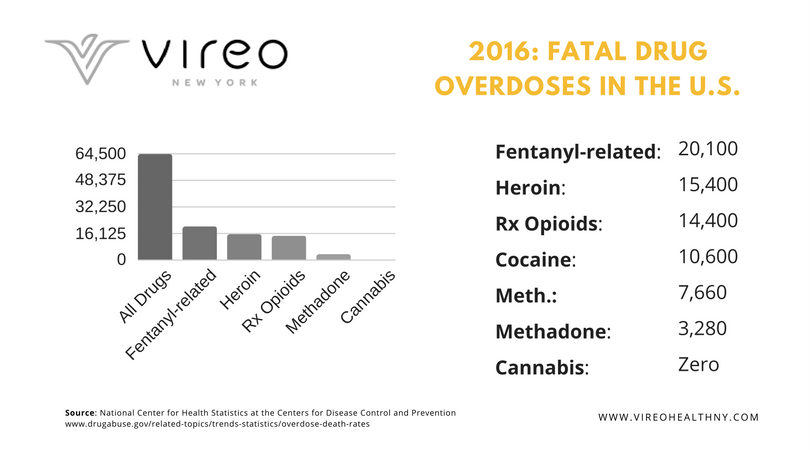
In 2017, when then-President Trump announced that opioid abuse amounted to a public health emergency, he was acknowledging a fact already sadly apparent to millions of Americans. The previous year, some 64,000 people died from drug overdoses (with prescription and illicit opioids responsible for the majority of drug overdoses). The most recent data, from 2021, showed that number had risen to over 80,000. For those Americans under the age of 50, drug overdose is now the leading cause of death.
With so many Americans dying each year from opioid overdoses, it’s more important than ever that we find a solution. But because such drugs tend to elicit such powerful dependance patterns among long-term users, that’s no simple task. In recent years, some clinicians have compared the upsides and downsides of cannabis vs opioids when it comes to addressing chronic pain.
While the findings aren’t unanimous, there’s now a strong case to be made that using cannabis for chronic pain is a far safer—and ultimately more sustainable—response both to the opioid crisis and one of its major causes: an epidemic of chronic pain.
In today’s post, we’ll explore some of the major questions around medical marijuana, treating chronic pain, and how we can turn the tide on this tragic trend.
Medical Marijuana for Chronic Pain: An Overview
Even a few years ago, chronic pain was thought of as a side effect of other, underlying medical conditions. While that’s true to an extent, this perception has begun to change. Given its persistence and how many lives are affected by it, a growing number of clinicians are framing chronic pain as a condition in and of itself.
Cannabis and opioids have both been used as a treatment for chronic pain throughout the years. And to better understand how either medicine interacts with chronic pain, we have to understand a little more about the phenomenon of pain itself. Because instead of there being a single type of pain, researchers now recognize no fewer than three major classes of pain:
- Nociceptive Pain: Resulting from a physical injury; often treated with anti-inflammatory medications such as NSAIDs.
- Neuropathic (or “Nerve”) Pain: Can also be caused by a physical injury, but refers specifically to a nerve injury. Doesn’t typically respond to NSAIDs.
- Central Pain: Sometimes called “mystery pain,” it occurs in the absence of a physical injury. One example is fibromyalgia, a condition that is both difficult to diagnose and treat.
Each of these major types of pain can range from mild to severe. This raises a question: Can medical marijuana treat chronic pain adequately enough to forgo opioids? Because cannabis is widely—and, we believe, correctly—perceived as being easier to tolerate than opioids, some chronic pain patients worry that it’s not strong enough to address chronic pain. Let’s tackle that question next.
Cannabis for Chronic Pain: Is it “Strong Enough” To Do the Job?
While cannabis is only now gaining re-acceptance in the medical field, it actually has a long and historic track record in terms of treating a variety of ailments. These days, clinical evidence clearly suggests that cannabis is far safer, less addictive, and less potentially destructive than opioids. But when comparing cannabis and opioids, can one actually treat chronic pain more effectively than the other? Let’s look at the available science.
A paper published in the Journal of Cannabis and Cannabinoid Research collected data from a group of 2,897 medical cannabis patients. It found that patients seem to prefer using cannabis in place of opioids:
- 34 percent reported having used opioid pain medication in the previous six months. A majority of patients reported that cannabis was just as effective or more effective than opioids, but without undesirable side effects.
- Of the patients who had previously used opioids, 97 percent reported having been able to reduce or eliminate them in favor of cannabis.
- Overall, 81 percent of patients reported that using cannabis alone was more effective than opioids.
The authors of the study concluded:
“Cannabis can be an effective treatment for pain, greatly reduces the chance of dependence, and eliminates the risk of fatal overdose compared to opioid-based medications. Medical cannabis patients report that cannabis is just as effective, if not more, than opioid-based medications for pain.”
Other studies corroborate these findings. A 2015 Harvard-led review of 28 previous studies examined the efficacy of cannabis for chronic pain and drew similar conclusions. The authors found that the use of marijuana for chronic pain, neuropathic pain, and spasticity due to multiple sclerosis is supported by high-quality evidence.
What about the safety profile of cannabis? A study by the University of Michigan found that cannabis, among other things:
- Decreased the side effects from other medications
- Improved subjects’ overall quality of life
- Reduced use of opioids, on average, by 64%
We should also point out that while opioid-induced fatal drug overdoses are only increasing, the Drug Enforcement Agency notes that no death from a cannabis overdose has ever been reported.
Medical Cannabis as an Alternative to Opioids
Evidence indicates that cannabis can reduce our dependence upon opioids. To underscore the point, in 2017 WeedMaps—a California company that publishes an online dispensary rating guide—launched a creative billboard marketing campaign. On a simple black background, the text read:
“States that legalized marijuana had 25% fewer opioid-related deaths.”
The message was stark and unforgettable, and it sparked heated controversy in neighborhoods hard hit by the opioid crisis. The WeedMaps data was based on a 2014 study published in JAMA Internal Medicine. In it the authors, Dr. Mark S. Brown and Marie J. Hayes, commented:
“The striking implication is that medical marijuana laws, when implemented, may represent a promising approach for stemming runaway rates of unintentional opioid-analgesic-related deaths.”
Cannabis vs Opioids: Use Throughout History
Both cannabis and opioids have both been used for many thousands of years to treat pain. Evidence indicates that cannabis has been used to treat chronic pain, stomach ailments, anxiety and a host of other conditions for at least 4,000 years. The medical uses of opium date back even further, to at least 3400 BCE. Although opium was recognized early for its powerful pain-killing properties, it was also understood to be habit-forming by at least the 18th century, if not long before.
By comparison, cannabis remained in the American pharmacopeia as an accepted folk remedy until the early 20th century. Unfortunately, the temperance movement and rising anti-immigrant sentiment—marijuana was linked with an influx of Mexican migrant workers—led to cannabis being banned in most states, and eventually on the federal level in 1937.As we pointed out earlier, research validates the vast amount of anecdotal evidence supporting the efficacy of cannabis in treating chronic pain. Given the relative safety of cannabis compared to opioid medications, from a public health perspective it seems clear: With a much lower risk of dependence than opioids and virtually no risk of fatal overdose, cannabis should be considered as a medically effective and far safer alternative.
Finding the Right Medical Marijuana for Chronic Pain
While cannabis can be a viable alternative to objectively harmful opioids, for some patients it requires a bit of trial and error to find the right cannabinoid ratio and intake method. That’s in part because cannabis is not a single drug but a highly complex plant with hundreds of cannabinoids and terpenes working together synergistically to influence its effects.
Here at Vireo Health, our research indicates that for chronic pain, most patients opt for products higher in THC. Dr. Stephen Dahmer, Vireo’s chief medical officer, had this to say when asked to comment on patients’ chronic pain experiences:
“What we’ve seen in chronic pain is that a patient will gravitate a little bit more towards a higher THC product. They’ll move in that direction if they’re not responding to the treatment that’s given. So, generally, in terms of dosing, we’ll slide them towards higher THC, but also increase the amount of CBD. That could potentiate [extend the duration of] the THC while offsetting potential side effects. In pain, most of the scientific research is going to back this up. If you look at the randomized double-blind control studies done specifically with neuropathic pain, it’s higher THC strains that have the best evidence behind them. But, we will also find in practicality if a patient is not responding to increasing levels of THC, sometimes we’ll flip things upside down and give them a high CBD, and particularly in inflammatory disorders, patients might respond well to that, where they may not respond well to a higher THC.
So, a combination of science and trial and error, and a lot of feedback. Very close feedback with the patient, making sure they’re getting the most optimal effects with the fewest side effects.”
While most patients seem to respond better to products with higher THC levels, others find a 1:1 (THC:CBD) or even a high-CBD product works well. Likewise, some people prefer inhalation, finding that vaporized or smoked cannabis delivers fast relief. Others find that inhalation to be unpleasant, and prefer oral administration in the form of capsules or tinctures.
Cannabis for Chronic Pain: Explore Vireo Health Today
There’s no “one size fits all” when it comes to cannabis medicine, but at Vireo we developed the Vireo Spectrum™ to make it easier to find the right cannabinoid profile for you. The products are color-coded correlating to the levels of THC and CBD, offering a simple visual cue as to which one will best address your symptoms and conditions.
What’s more, we have a whole team of experts at every Vireo location who are available to support you in your journey to find the right medical marijuana product for you. Do you have any further questions about cannabis for chronic pain or any other topics related to marijuana as medicine? Don’t hesitate to reach out. We’re always here to help.